Secondary Hypertension
Secondary hypertension accounts for approximately 5-10% of all cases of hypertension, with the remaining being primary hypertension. Secondary hypertension has an identifiable cause, whereas primary hypertension has no known cause (idiopathic).
There are many known conditions that can cause secondary hypertension. Regardless of the cause, arterial pressure becomes elevated because of an increase in cardiac output, an increase in systemic vascular resistance, or both. When cardiac output is elevated, it is because of either increased neurohumoral activation of the heart or increased blood volume. Increased systemic vascular resistance is most commonly caused, at least initially, by increased sympathetic activation or by the effects of circulating vasoconstrictors (e.g., angiotensin II). Anatomic considerations, such as narrowing of the aorta (e.g., coarctation) or chronic changes in vascular structure (e.g., vascular hypertrophy) can also cause or contribute to increased systemic vascular resistance.
Patients with secondary hypertension are best treated by controlling or removing the underlying disease or pathology, although they may still require antihypertensive drugs.
Some causes for secondary hypertension are listed below:
- Renal artery stenosis
- Chronic renal disease
- Primary hyperaldosteronism
- Stress
- Sleep apnea
- Hyper- or hypothyroidism
- Pheochromocytoma
- Preeclampsia
- Aortic coarctation
Renal artery stenosis (renovascular disease)
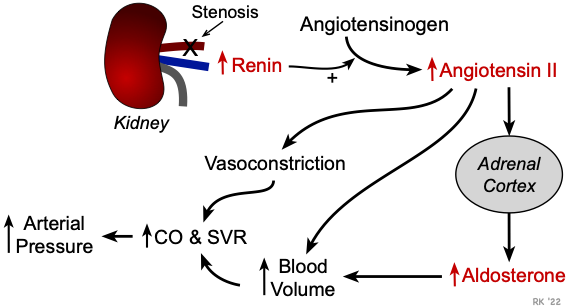 Renal artery disease can cause narrowing of the vessel lumen (stenosis). The reduced lumen diameter decreases the pressure at the afferent arteriole in the kidney and reduces renal perfusion. This stimulates renin release by the kidney, which increases circulating angiotensin II (AII) and aldosterone. These hormones increase blood volume by enhancing renal reabsorption of sodium and water, which increases cardiac output (CO) by the Frank-Starling mechanism. Increased AII also causes systemic vasoconstriction (SVR) and enhances sympathetic activity, and chronic elevation of AII promotes cardiac and vascular hypertrophy. Therefore, hypertension caused by renal artery stenosis results from both an increase in systemic vascular resistance and an increase in cardiac output.
Renal artery disease can cause narrowing of the vessel lumen (stenosis). The reduced lumen diameter decreases the pressure at the afferent arteriole in the kidney and reduces renal perfusion. This stimulates renin release by the kidney, which increases circulating angiotensin II (AII) and aldosterone. These hormones increase blood volume by enhancing renal reabsorption of sodium and water, which increases cardiac output (CO) by the Frank-Starling mechanism. Increased AII also causes systemic vasoconstriction (SVR) and enhances sympathetic activity, and chronic elevation of AII promotes cardiac and vascular hypertrophy. Therefore, hypertension caused by renal artery stenosis results from both an increase in systemic vascular resistance and an increase in cardiac output.
Chronic renal disease
Pathologic processes (e.g., diabetic nephropathy, glomerulonephritis) can damage nephrons in the kidney. When this occurs, the kidney cannot excrete normal amounts of sodium, which leads to sodium and water retention, increased blood volume, and increased cardiac output by the Frank-Starling mechanism. Renal disease may also result in increased release of renin, leading to a renin-dependent form of hypertension, as described above. The elevation in arterial pressure secondary to renal disease can be viewed as an attempt by the kidney to increase renal perfusion and restore glomerular filtration.
Primary hyperaldosteronism
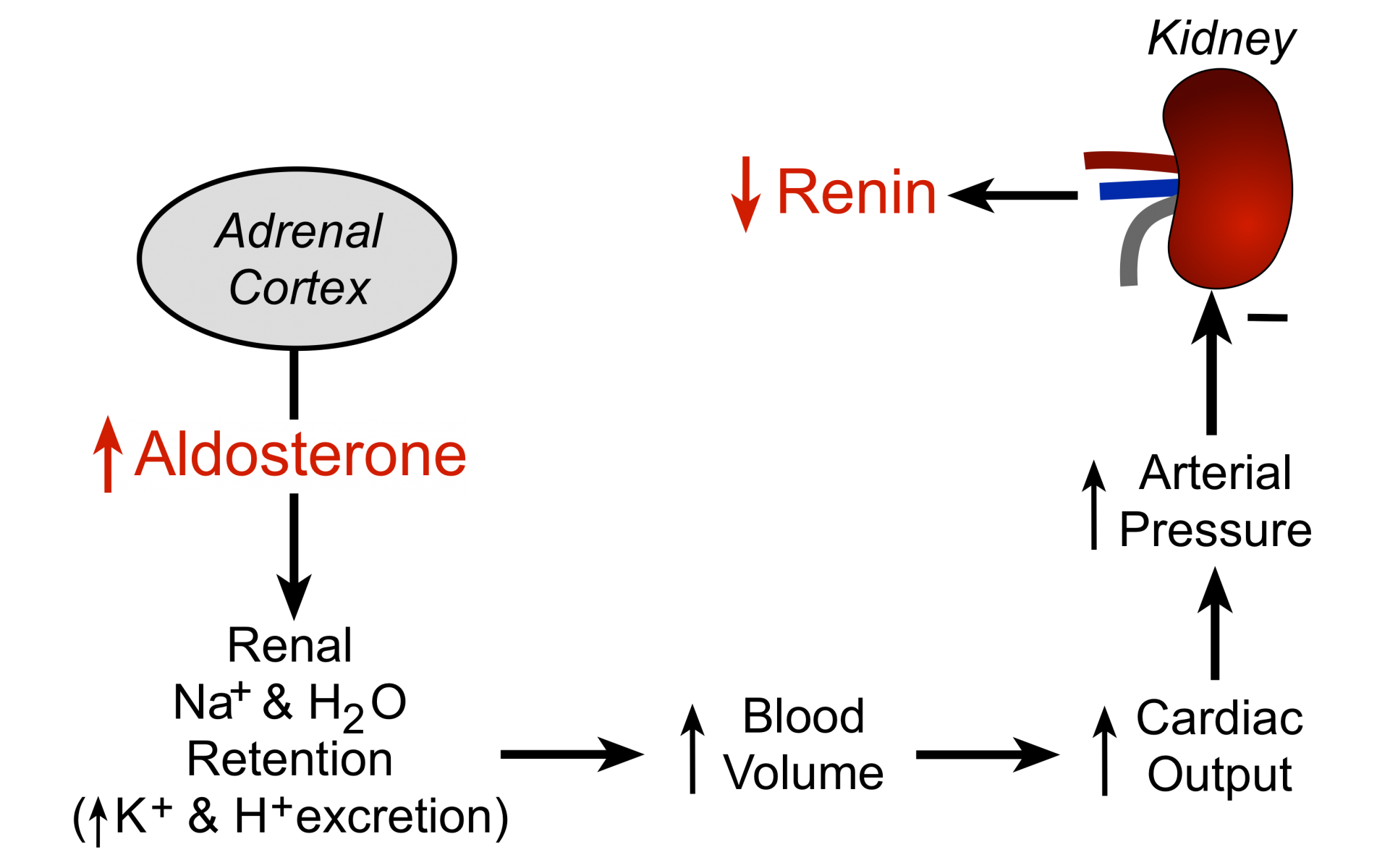 An adrenal adenoma or adrenal hyperplasia may cause abnormal secretion of aldosterone. Increased circulating aldosterone causes renal retention of sodium and water (see figure), which causes blood volume and arterial pressure to increase. Plasma renin levels are usually decreased as the body attempts to suppress the renin-angiotensin system; there is also hypokalemia associated with the high levels of aldosterone.
An adrenal adenoma or adrenal hyperplasia may cause abnormal secretion of aldosterone. Increased circulating aldosterone causes renal retention of sodium and water (see figure), which causes blood volume and arterial pressure to increase. Plasma renin levels are usually decreased as the body attempts to suppress the renin-angiotensin system; there is also hypokalemia associated with the high levels of aldosterone.
Stress
Emotional stress leads to activation of the sympathetic nervous system, which causes increased release of norepinephrine from sympathetic nerves in the heart and blood vessels, leading to increased cardiac output and increased systemic vascular resistance. The adrenal medulla secretes more catecholamines (epinephrine and norepinephrine) in response to stress. Activation of the sympathetic nervous system increases circulating angiotensin II, aldosterone, and vasopressin, which can increase systemic vascular resistance and blood volume. Prolonged elevation of angiotensin II and catecholamines can lead to cardiac and vascular hypertrophy, both of which can contribute to a sustained increase in blood pressure.
Sleep Apnea
Sleep apnea is a disorder in which people repeatedly cease breathing for short periods of time (10–30 seconds) during their sleep. This condition is often associated with obesity, although it can have other causes, such as airway obstruction or disorders of the central nervous system. These individuals have a higher incidence of hypertension. The mechanism of hypertension may be related to sympathetic activation and hormonal changes associated with repeated periods of apnea-induced hypoxia and hypercapnia, and from stress associated with the loss of sleep.
Hyper- or hypothyroidism
Both hyperthyroidism and hypothyroidism can lead to hypertension in some patients, although the mechanisms are poorly understood. Elevated thyroxin levels cause increased blood volume through activation of the renin-angiotensin-aldosterone system, and increased heart rate and ventricular contractility. Recent studies suggest cardiac changes are independent of sympathetic adrenergic activity. Subnormal thyroxin levels (hypothyroidism) reduce tissue metabolism, which may decrease the production of tissue vasodilator metabolites and endothelial production of nitric oxide, and cause vasoconstriction and increased arterial pressure. There is also an increase in arterial stiffness (reduced arterial compliance).
Pheochromocytoma
Catecholamine secreting tumors in the adrenal medulla can lead to very high levels of circulating catecholamines (both epinephrine and norepinephrine). This leads to alpha-adrenoceptor mediated systemic vasoconstriction and beta-adrenoceptor mediated cardiac stimulation, both of which contribute to significant elevations in arterial pressure. Despite the elevation in arterial pressure, tachycardia occurs because of the direct effects of the catecholamines on the heart and vasculature. Excessive beta-adrenoceptor stimulation in the heart often leads to arrhythmias. Pheochromocytoma is diagnosed by measuring plasma or urine catecholamine levels and their metabolites (vanillylmandelic acid and metanephrine).
Preeclampsia
This is a serious condition that sometimes develops during the third trimester of pregnancy that causes hypertension due to increased blood volume, which increases cardiac output by the Frank-Starling mechanism. The condition usually disappears after parturition.
Aortic coarctation
Coarctation (narrowing) of the aorta is a congenital defect that most commonly is found just distal to the left subclavian artery in the aortic arch. Obstruction of the aorta at this point reduces distal arterial pressures and elevates arterial pressures in the head and arms. The reduced systemic arterial pressure activates the renin-angiotensin-aldosterone system, which leads to an increase in blood volume, which further increases arterial pressures in the upper body and may largely offset the reduction in lower body arterial pressures. This condition is readily diagnosed by comparing arterial pressures measured in the arms and legs. Normally, these pressures are very similar, but with coarctation, arterial pressures in the arms can be much greater than arterial pressures measured in the legs. Because this is a chronic condition, the baroreceptors are desensitized, and upper body arterial pressures remain elevated because of the increased cardiac output to these parts of the body.
Revised 11/03/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)