Blood Volume
Blood volume is determined by the amount of water and sodium ingested, excreted by the kidneys into the urine, and lost through the gastrointestinal tract, lungs and skin. The amounts of water and sodium ingested and lost are highly variable. To maintain blood volume within a normal range, the kidneys regulate the amount of water and sodium lost into the urine. For example, if excessive water and sodium are ingested, the kidneys normally respond by excreting more water and sodium into the urine. The details of how the kidneys handle water and sodium are beyond the scope of this cardiovascular website; therefore, the reader is encouraged to consult general medical physiology textbooks to learn more about this topic. The following paragraphs briefly summarize how renal excretion of water and sodium are regulated and how blood volume affects cardiovascular function.
Regulation of Blood Volume by Renal Excretion of Water and Sodium
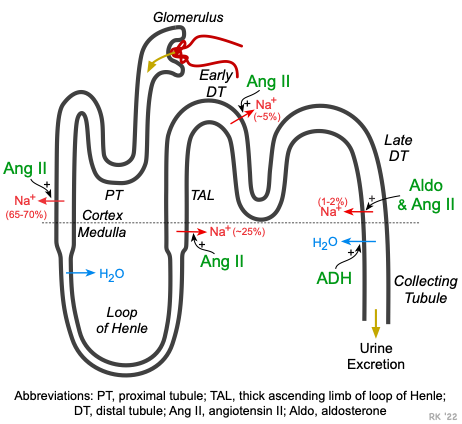 Blood is filtered at the glomerulus. This filtrate contains water, sodium, and other substances. As the filtrate travels through the proximal tubule, loop of Henle, distal and collecting tubules, the concentration of sodium is altered by transport of sodium across the tubular wall and into the renal interstitium, where it can diffuse into a dense network of intrarenal capillaries. Some of the renal tubules are permeable to water, so water leaves those tubular regions along with the sodium.
Blood is filtered at the glomerulus. This filtrate contains water, sodium, and other substances. As the filtrate travels through the proximal tubule, loop of Henle, distal and collecting tubules, the concentration of sodium is altered by transport of sodium across the tubular wall and into the renal interstitium, where it can diffuse into a dense network of intrarenal capillaries. Some of the renal tubules are permeable to water, so water leaves those tubular regions along with the sodium.
The primary mechanism by which the kidneys regulate blood volume is by adjusting the amount of water and sodium lost into the urine. At different sites along the proximal tubules, thick ascending limb of the loop of Henle, and distal and collecting tubules, sodium transport is regulated by angiotensin II (Ang II), which increases sodium transport, leading to sodium retention. In the collecting tubules, another hormone (aldosterone), stimulates sodium transport from the tubular fluid into the interstitium. Together, Ang II and aldosterone provide a powerful mechanism for increasing sodium retention and consequently fluid volume in the body. A third hormone, antidiuretic hormone (ADH), increases water permeability in the late distal tubules and collecting tubules. This enables water to diffuse from the tubular fluid into the hypertonic interstitium, thereby reducing urine volume and water loss. Besides these hormone actions on sodium transport and water movement, changes in renal blood flow and glomerular filtration can affect the amount of sodium and water filtered at the glomerulus and entering the renal tubules. For example, increased blood volume increases arterial pressure, renal perfusion, and glomerular filtration rate. This leads to an increase in renal excretion of water and sodium, that is termed pressure natriuresis. In certain types of renal disease, the pressure natriuresis relationship is altered so that the kidneys retain more sodium and water at a given arterial pressure, increasing blood volume.
Activation of the renin-angiotensin-aldosterone (RAAS) system causes increased sodium retention by the kidneys, which leads to reduced water loss into the urine and therefore blood volume expansion. RAAS activation occurs during heart failure, which leads to fluid retention in the body. RAAS activation also occurs with renal artery stenosis, which is one cause of secondary hypertension. Drugs that block the formation of angiotensin II (i.e., angiotensin converting enzyme inhibitors), or block aldosterone receptors (e.g., spironolactone) enhance sodium and water loss, and thereby reduce blood volume. Therefore, any mechanism or drug that alters RAAS activity will affect blood volume.
How Blood Volume Affects Blood Pressure
Changes in blood volume affect arterial pressure by changing cardiac output. An increase in blood volume increases central venous pressure. This increases right atrial pressure, right ventricular end-diastolic pressure and volume. This increase in ventricular preload increases ventricular stroke volume by the Frank-Starling mechanism. An increase in right ventricular stroke volume increases pulmonary venous blood flow to the left ventricular, increasing left ventricular preload and stroke volume. An increase in stroke volume then increases cardiac output and arterial blood pressure.
Revised 12/06/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)