Effects of Gravity on Venous Return
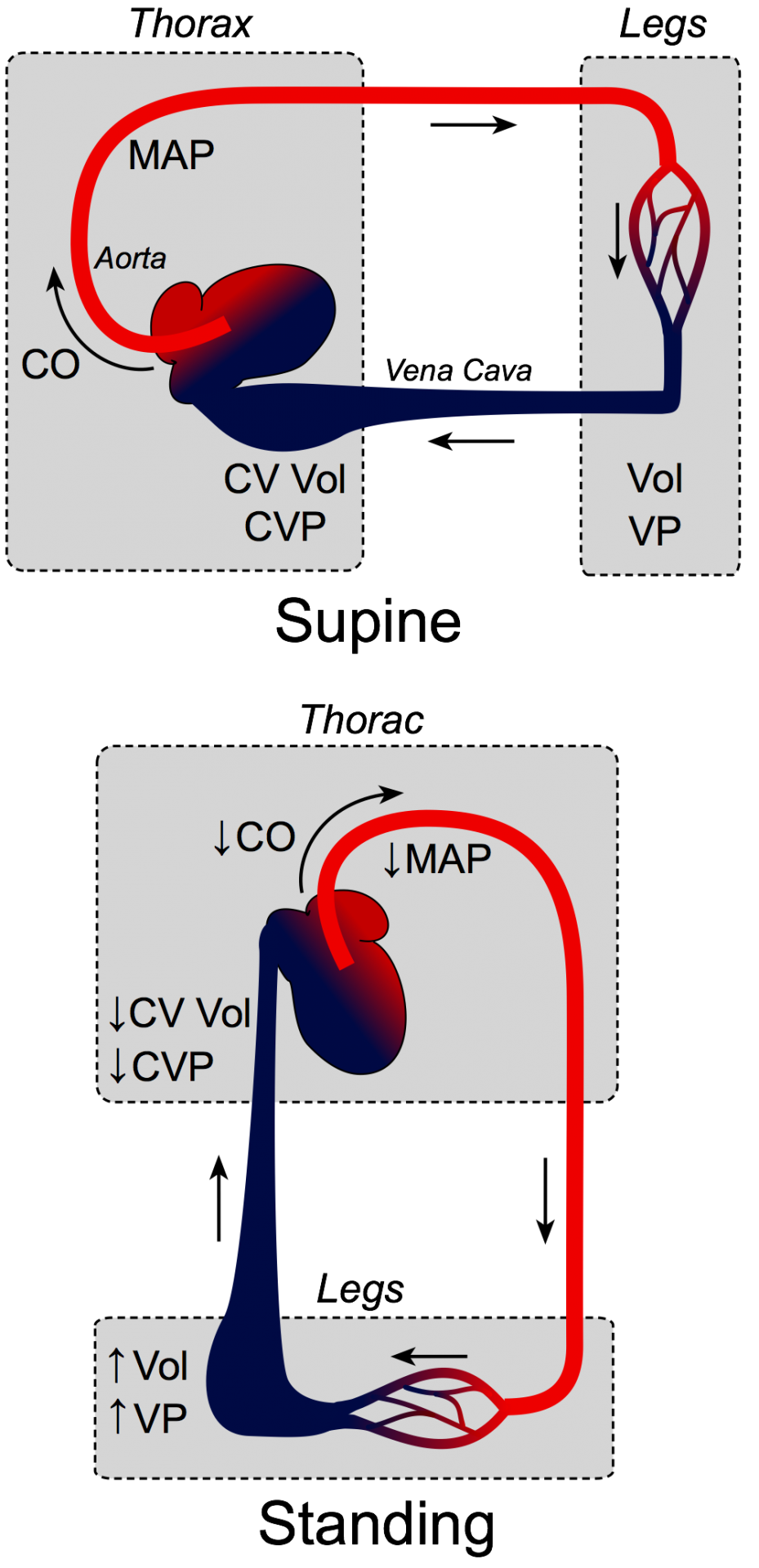 Gravitational forces significantly affect venous return, cardiac output, and arterial and venous pressures. To illustrate this, consider a person who is lying down and then suddenly stands up. When the person is lying down (supine position), gravitational forces are similar on the thorax, abdomen, and legs because these compartments lie in the same horizontal plane. In this position, venous blood volumes and pressures are distributed evenly throughout the body. When the person suddenly stands upright, gravity acts on the vascular volume, causing blood to accumulate in the lower extremities. (Compare the size of veins on the top of your feet while lying down and standing.) Because venous compliance is high and the veins readily expand with blood, most of the blood volume shift occurs in the veins. Therefore, venous volume (Vol) and pressure (VP) become very high in the feet and lower limbs when standing. This shift in blood volume decreases thoracic venous blood volume (CV Vol) and, therefore, central venous pressure (CVP) decreases. This decreases right ventricular filling pressure (preload), leading to a decline in stroke volume by the Frank-Starling mechanism. Left ventricular stroke volume also falls because of reduced pulmonary venous return (decreased left ventricular preload). This causes cardiac output (CO) and mean arterial pressure (MAP) to fall. If arterial pressure falls appreciably upon standing, this is termed orthostatic or postural hypotension. This fall in arterial pressure can reduce cerebral blood flow to where a person might experience syncope (fainting).
Gravitational forces significantly affect venous return, cardiac output, and arterial and venous pressures. To illustrate this, consider a person who is lying down and then suddenly stands up. When the person is lying down (supine position), gravitational forces are similar on the thorax, abdomen, and legs because these compartments lie in the same horizontal plane. In this position, venous blood volumes and pressures are distributed evenly throughout the body. When the person suddenly stands upright, gravity acts on the vascular volume, causing blood to accumulate in the lower extremities. (Compare the size of veins on the top of your feet while lying down and standing.) Because venous compliance is high and the veins readily expand with blood, most of the blood volume shift occurs in the veins. Therefore, venous volume (Vol) and pressure (VP) become very high in the feet and lower limbs when standing. This shift in blood volume decreases thoracic venous blood volume (CV Vol) and, therefore, central venous pressure (CVP) decreases. This decreases right ventricular filling pressure (preload), leading to a decline in stroke volume by the Frank-Starling mechanism. Left ventricular stroke volume also falls because of reduced pulmonary venous return (decreased left ventricular preload). This causes cardiac output (CO) and mean arterial pressure (MAP) to fall. If arterial pressure falls appreciably upon standing, this is termed orthostatic or postural hypotension. This fall in arterial pressure can reduce cerebral blood flow to where a person might experience syncope (fainting).
When a person stands up, baroreceptor reflexes are rapidly activated to restore arterial pressure (primarily through systemic vasoconstriction) so that mean arterial pressure normally is not reduced by more than a few mmHg when a person is standing compared to lying down. However, to maintain this normal mean arterial pressure, the person who is standing upright has increased systemic vascular resistance (sympathetic mediated), decreased venous compliance (because of sympathetic activation of veins), decreased stroke volume (due to decreased preload), and increased heart rate (baroreceptor-mediated tachycardia). Patients with autonomic nerve dysfunction or hypovolemia may not effectively use these compensatory mechanisms and therefore will display orthostatic hypotension.
Without the operation of important compensatory mechanisms, standing upright would lead to significant edema in the feet and lower legs besides orthostatic hypotension. Venous pooling and reduced venous return are rapidly compensated in a normal individual by neurogenic vasoconstriction of veins, the functioning of venous valves, by muscle pump activity, and by the abdominothoracic pump. When these mechanisms are operating, capillary and venous pressures in the feet will only be elevated by 10-20 mmHg, mean aortic pressure will be maintained, and central venous pressure will be only slightly reduced.
When a standing person suddenly changes to the supine position, the blood volume in the thoracic (central venous) compartment increases as blood volume shifts from the legs to the thorax. This increases preload on the heart, increasing stroke volume, although the resulting increase in cardiac output will be tempered by a reduction in heart rate through vagal activation and sympathetic withdrawal (baroreflex). Sympathetic activation of the systemic vasculature is also reduced, which causes systemic vascular resistance to fall as the resistance vessels dilate.
Revised 02/01/2024

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)