Valvular Stenosis
Stenosis of atrioventricular valves (tricuspid, mitral) or outflow tract valves (pulmonic, aortic) leads to an elevated pressure gradient across the valve as blood is flowing through the valve opening. This increased pressure gradient results from an increase in the pressure proximal to the valve and a small fall in pressure distal to the valve. The magnitude of the pressure gradient depends on the severity of the stenosis and the flow rate across the valve. A narrowed valve also increases the velocity of the blood as it travels across the valve, which can cause turbulence and a heart murmur.
Mitral and tricuspid valve stenosis
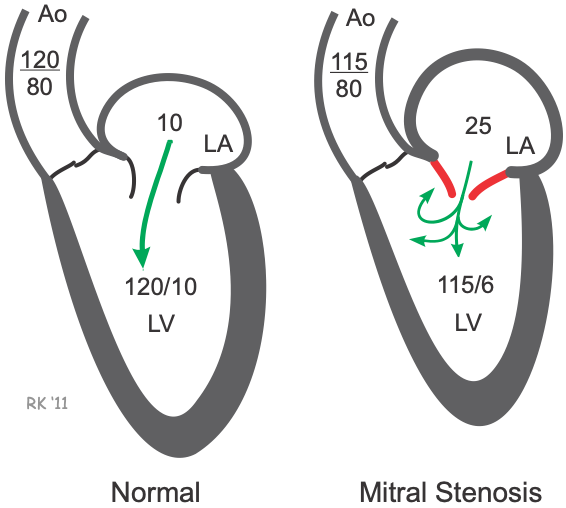 Mitral valve stenosis results from a narrowing of the opened mitral valve orifice so that it is more difficult for blood to flow from the left atrium (LA) into the left ventricle (LV) during ventricular diastole (see figure). The high resistance across the stenotic mitral valve causes blood to back up into the left atrium, increasing LA pressure, which in this example is 25 mmHg (normally ~10 mmHg). This results in the LA pressure being much greater than the LV pressure during diastolic filling. If left ventricular maximal filled volume (end-diastolic volume) is reduced despite the elevated left atrial pressure, then the left ventricular end-diastolic pressure will be reduced as shown in the figure (6 mmHg compared to 10 mmHg in the normal heart). The left atrium enlarges (hypertrophies) over time because it has to generate higher than normal pressures when it contracts against the high resistance of the stenotic valve. The reduced ventricular filling (decreased preload) decreases ventricular stroke volume by the Frank-Starling mechanism. If stroke volume falls significantly, the decreased cardiac output may reduce aortic pressure (AP; 115/80 mmHg in this example), although compensatory mechanisms (e.g., systemic vasoconstriction) will attempt to maintain normal arterial pressure. Mitral valve stenosis is associated with a diastolic murmur because of turbulence that occurs as blood flows across the stenotic valve.
Mitral valve stenosis results from a narrowing of the opened mitral valve orifice so that it is more difficult for blood to flow from the left atrium (LA) into the left ventricle (LV) during ventricular diastole (see figure). The high resistance across the stenotic mitral valve causes blood to back up into the left atrium, increasing LA pressure, which in this example is 25 mmHg (normally ~10 mmHg). This results in the LA pressure being much greater than the LV pressure during diastolic filling. If left ventricular maximal filled volume (end-diastolic volume) is reduced despite the elevated left atrial pressure, then the left ventricular end-diastolic pressure will be reduced as shown in the figure (6 mmHg compared to 10 mmHg in the normal heart). The left atrium enlarges (hypertrophies) over time because it has to generate higher than normal pressures when it contracts against the high resistance of the stenotic valve. The reduced ventricular filling (decreased preload) decreases ventricular stroke volume by the Frank-Starling mechanism. If stroke volume falls significantly, the decreased cardiac output may reduce aortic pressure (AP; 115/80 mmHg in this example), although compensatory mechanisms (e.g., systemic vasoconstriction) will attempt to maintain normal arterial pressure. Mitral valve stenosis is associated with a diastolic murmur because of turbulence that occurs as blood flows across the stenotic valve.
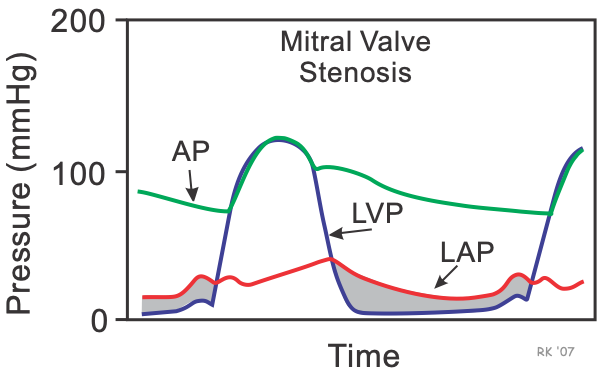 Mitral stenosis affects left atrial pressure (LAP), aortic pressure (AP) and left ventricular pressure (LVP) during the cardiac cycle. The shaded area separating the LAP from the LVP during diastole represents the elevated pressure gradient that is characteristic of mitral stenosis. The gradient is highest during early diastole, when the flow across the valve is highest. Normally, the pressure gradient is small (a few mmHg); however, the pressure gradient can become quite high during severe stenosis (10-30 mmHg). The increase in LA pressure can cause pulmonary congestion and edema because of increased pulmonary capillary hydrostatic pressure.
Mitral stenosis affects left atrial pressure (LAP), aortic pressure (AP) and left ventricular pressure (LVP) during the cardiac cycle. The shaded area separating the LAP from the LVP during diastole represents the elevated pressure gradient that is characteristic of mitral stenosis. The gradient is highest during early diastole, when the flow across the valve is highest. Normally, the pressure gradient is small (a few mmHg); however, the pressure gradient can become quite high during severe stenosis (10-30 mmHg). The increase in LA pressure can cause pulmonary congestion and edema because of increased pulmonary capillary hydrostatic pressure.
The changes in ventricular pressures and volumes that result from mitral stenosis can be illustrated using pressure-volume loops.
An 8-minute recorded lecture describing mitral stenosis can be viewed by clicking on Mitral Stenosis Pathophysiology.
Tricuspid valve stenosis is similar to mitral valve stenosis, except that the pressure and volume changes occur on the right side of the heart.
Aortic and pulmonic valve stenosis
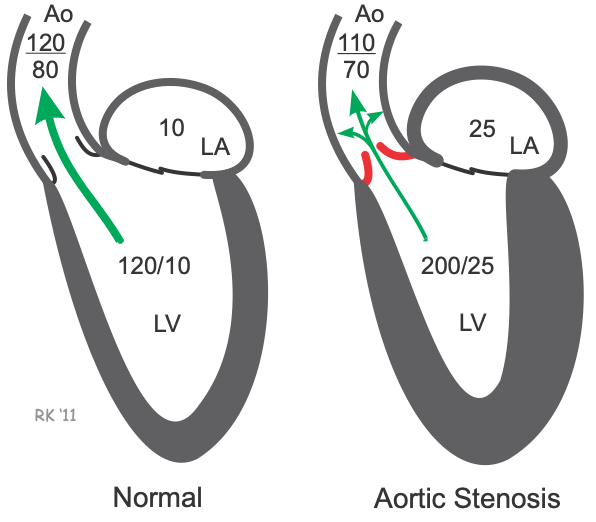 Aortic valve stenosis is characterized by the left ventricular pressure being much greater than aortic pressure during left ventricular (LV) ejection. In the figure, LV peak systolic pressure during ejection is 200 mmHg (normally ~120 mmHg) and the aortic pressure is reduced from 120 to 110 mmHg. Normally, the pressure gradient across the aortic valve during ejection is small (a few mmHg); however, the pressure gradient can become quite high (>100 mmHg) during severe stenosis. The elevated pressure gradient across the stenotic valve results from both increased resistance (related to narrowing of the valve opening) and turbulence distal to the valve. Increased flow across the valve enhances the magnitude of the pressure gradient (e.g., during exercise).
Aortic valve stenosis is characterized by the left ventricular pressure being much greater than aortic pressure during left ventricular (LV) ejection. In the figure, LV peak systolic pressure during ejection is 200 mmHg (normally ~120 mmHg) and the aortic pressure is reduced from 120 to 110 mmHg. Normally, the pressure gradient across the aortic valve during ejection is small (a few mmHg); however, the pressure gradient can become quite high (>100 mmHg) during severe stenosis. The elevated pressure gradient across the stenotic valve results from both increased resistance (related to narrowing of the valve opening) and turbulence distal to the valve. Increased flow across the valve enhances the magnitude of the pressure gradient (e.g., during exercise).
Aortic stenosis can reduce ventricular stroke volume due to increased afterload (which decreases ejection velocity). The reduced stroke volume decreases the aortic pulse pressure, and the mean aortic pressure falls if the reduced cardiac output is not offset by an increase in systemic vascular resistance.
Because the ventricle is required to generate greater pressures, this leads to ventricular hypertrophy (thickening of the muscular walls) and diastolic dysfunction (impaired filling). Hypertrophied ventricles are less compliant and therefore have a higher filling pressure at a given end-diastolic volume (the end-diastolic pressure is 25 mmHg in this example). Elevated left ventricular end-diastolic pressure causes blood to back up into the left atrium and pulmonary veins, which increases left atrial pressure (and pulmonary capillary wedge pressure). This enlarges the left atrium and results in hypertrophy of the atrial wall because the left atrium has to generate increased pressure when it contracts. Aortic valve stenosis is associated with a mid-systolic murmur because of turbulence that occurs as blood flows across the stenotic valve.
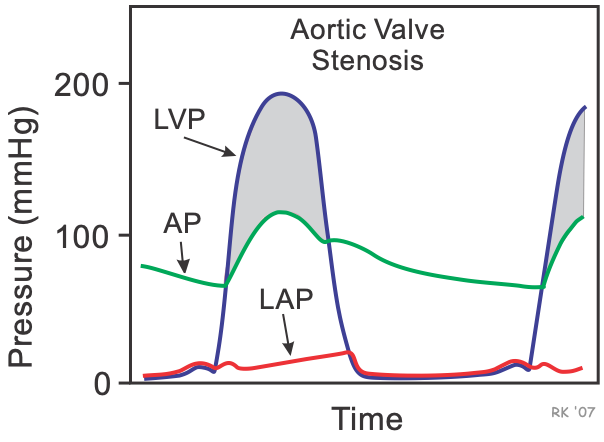 Aortic stenosis alters left ventricular pressure (LVP), aortic pressure (AP) and left atrial pressure (LAP) during the cardiac cycle. The shaded area separating the LVP from the AP during systole represents the elevated pressure gradient that is characteristic of aortic stenosis. Note that the gradient only occurs during the time that blood is being ejected across the stenotic valve. Such measurements of LVP and AP by cardiac catheterization provide a quantitative, hemodynamic assessment of the severity of stenosis.
Aortic stenosis alters left ventricular pressure (LVP), aortic pressure (AP) and left atrial pressure (LAP) during the cardiac cycle. The shaded area separating the LVP from the AP during systole represents the elevated pressure gradient that is characteristic of aortic stenosis. Note that the gradient only occurs during the time that blood is being ejected across the stenotic valve. Such measurements of LVP and AP by cardiac catheterization provide a quantitative, hemodynamic assessment of the severity of stenosis.
Changes in ventricular pressures and volumes that result from aortic stenosis can be illustrated using pressure-volume loops.
An 18-minute recorded lecture describing aortic stenosis can be viewed by clicking on Aortic Stenosis Pathophysiology.
Pulmonic valve stenosis is analogous to aortic valve stenosis, except that the changes in pressure are on the right side of the heart. A pressure gradient occurs across the pulmonic valve during right ventricular ejection. Compensatory increases in right ventricular end-diastolic pressure and right atrial pressure and volume occur; however, the pressure changes are generally less than what is observed on the left side of the heart.
Revised 11/07/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)