Peripheral Arterial Occlusive Disease
Peripheral arterial occlusive disease (PAOD) results either from atherosclerotic or inflammatory processes causing lumen narrowing (stenosis), or from thrombus formation (usually associated with underlying atherosclerotic disease). When these conditions arise, there is an increase in vessel resistance that can lead to a reduction in distal artery pressure and blood flow. The following discussion assumes chronic atherosclerotic conditions in the human lower limb that result in stenotic lesions. The hemodynamics and underlying mechanisms of PAOD in the human limb are very similar to what is found in coronary artery disease.
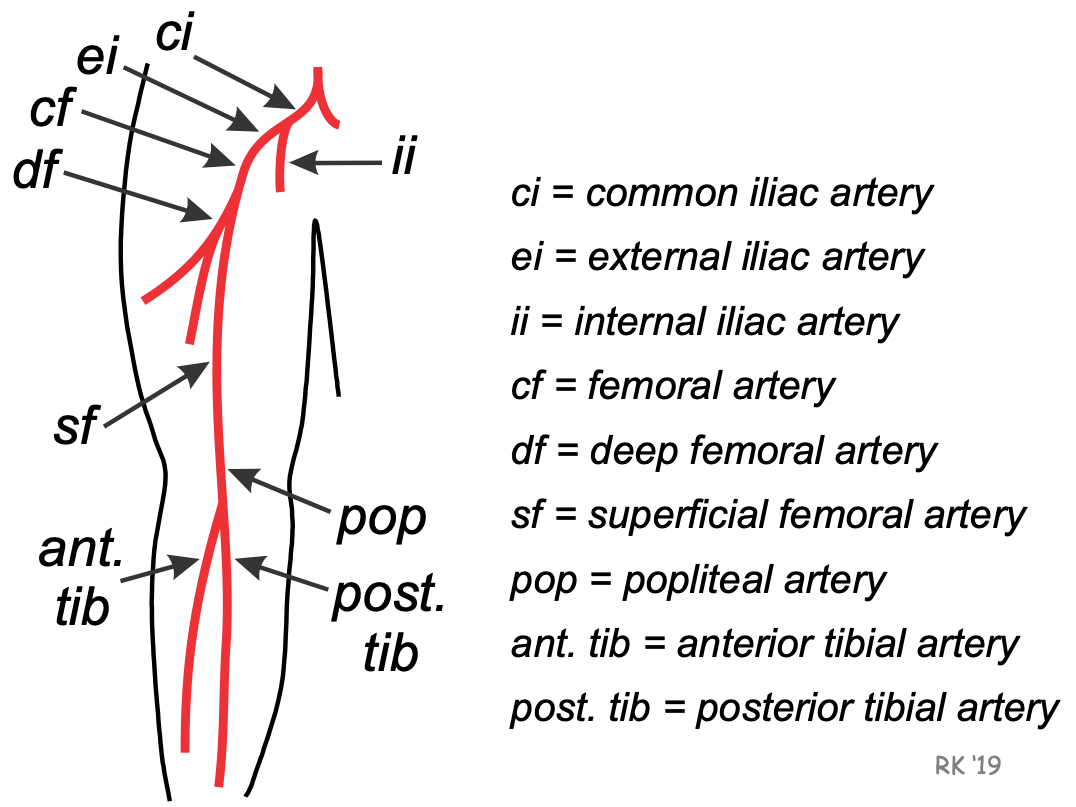 A common site for PAOD is in the leg (see figure). The circulation to the leg is derived from the common femoral artery, that is a continuation of the external iliac artery. The common femoral artery branches into the deep femoral and superficial femoral arteries. The deep femoral supplies blood flow to the thigh, and receives approximately 70% of the common femoral artery flow. The superficial femoral artery continues down the leg and becomes the popliteal artery just above the knee. Two major arteries at the termination of the popliteal artery are the anterior and posterior tibial arteries, which supply blood flow to the lower leg and foot.
A common site for PAOD is in the leg (see figure). The circulation to the leg is derived from the common femoral artery, that is a continuation of the external iliac artery. The common femoral artery branches into the deep femoral and superficial femoral arteries. The deep femoral supplies blood flow to the thigh, and receives approximately 70% of the common femoral artery flow. The superficial femoral artery continues down the leg and becomes the popliteal artery just above the knee. Two major arteries at the termination of the popliteal artery are the anterior and posterior tibial arteries, which supply blood flow to the lower leg and foot.
The process of atherosclerosis causes intimal thickening and plaque formation, which decreases the effective radius of the afflicted arterial segment. Although atherosclerosis is a diffuse process affecting all the arteries, some arterial segments in the limb often undergo greater stenosis than others do. Therefore, it is common to find stenotic lesions associated with specific arteries (e.g., external iliac, common femoral and superficial femoral arteries).
Based on Poiseuille's equation, a decrease in vessel radius increases resistance to the fourth power of the change in radius. Therefore, a 50% reduction in radius (one-half normal radius) will cause the resistance to increase by a factor of 16. Hemodynamically, this would cause flow to decrease by a factor of 16 assuming the perfusion pressure is constant, laminar flow conditions prevail, and that the resistance of this segment represents the total resistance to flow (i.e., the segment is not one of multiple in-series segments). However, because the major arteries of the limb circulation have series and parallel branches, a stenotic lesion has to have its radius decreased by over 60% to result in a significant hemodynamic effect (i.e., critical stenosis). For any reduction in radius, the longitudinal pressure drop across the length of the lesion will be significantly augmented if turbulence occurs.
PAOD can lead to limb ischemia. In mild-to-moderate PAOD, the increased resistance to flow will lead to decreased maximal flow capacity during limb exercise (i.e., decreased active hyperemia). This can cause ischemic pain during exercise that is termed intermittent claudication. The pain is caused by tissue hypoxia resulting from a high oxygen demand that is not met by an adequate increase in oxygen delivery (i.e., increased blood flow). In other words, there is a reduction in the oxygen supply/demand ratio. Metabolites formed under anaerobic conditions in the muscle can stimulate pain receptors in the muscle. Inadequate oxygen supply during exercise can also lead to muscle weakness and fatigue.
Stenotic arterial lesions may or may not alter resting blood flow. Atherosclerosis is a disease process that occurs over years. The circulation distal to a stenotic lesion often undergoes collateralization, which reduces resistance and helps to maintain normal resting blood flow despite a reduced perfusion pressure. Even acute reductions in perfusion pressure lead to a fall in distal vascular resistance and normalization of blood flow by the mechanism of autoregulation.
CLICK HERE to learn more about the hemodynamics associated with single and multiple stenotic lesions in the limb circulation.
Revised 01/30/2023

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)