Systemic Circulation
Vascular Network
The left ventricle ejects blood into the aorta, which then distributes the blood flow throughout the body using a network of blood vessels. Just beyond the aortic valve in the ascending aorta, there are small openings (left and right coronary ostia) from which arise the left and right coronary arteries that supply blood flow to the heart muscle. Near the top of the aortic arch, there are three major arteries that distribute blood flow to the upper thorax, arms and head. The first is the brachiocephalic artery, which shortly branches into the right subclavian artery (supplies the upper thorax, right arm and head) and the right common carotid artery (supplies the head). The next branch from the aortic arch is the left common carotid artery, which also supplies the head. The third major artery arising from the aortic arch is the left subclavian artery, which supplies blood flow to the upper thorax, left arm and head. Past the arch, the aorta descends downward (descending aorta) through the thorax (thoracic aorta) where it gives off several small arterial vessels to supply blood flow to the thorax. When the aorta passes through the diaphragm, it continues as the abdominal aorta. Several major arteries branch from the abdominal aorta, including those that supply blood to the visceral organs (e.g., stomach, intestines, kidneys). In the lower abdomen, the aorta bifurcates into the left and right common iliac arteries, which supply blood to the pelvic region and the legs via additional bifurcations and branches.
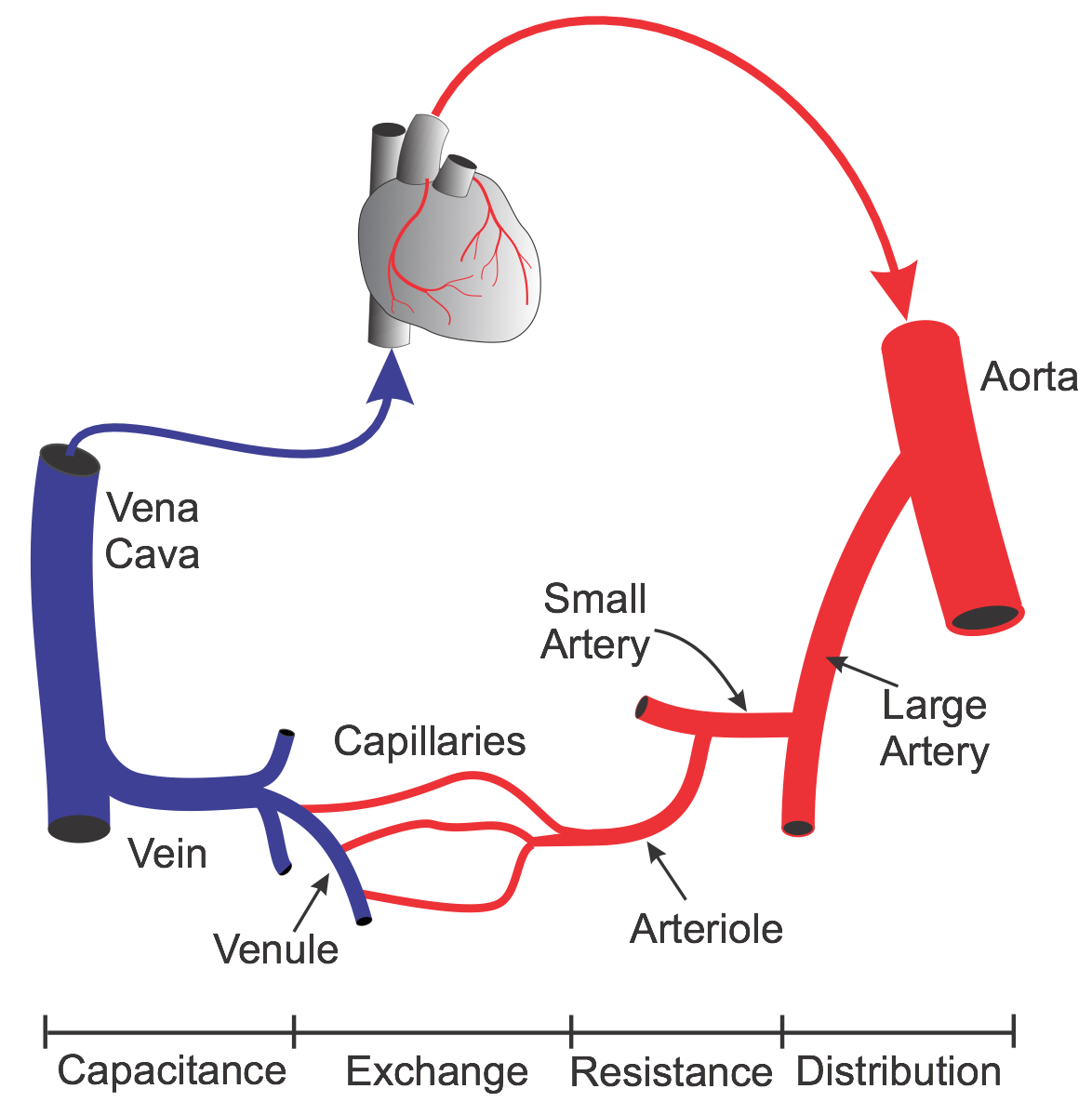 The aorta, besides being the main vessel to distribute blood to the arterial system, dampens the pulsatile pressure that results from the intermittent outflow from the left ventricle. The actual dampening is a function of aortic compliance. Large arteries branching off the aorta (e.g., carotid, mesenteric, renal arteries) distribute the blood flow to specific organs. These large arteries, although capable of constricting and dilating, play only a small role in regulating pressure and blood flow under normal physiological conditions. Once a large artery reaches the organ it supplies, it branches into small arteries that distribute blood flow within the organ. These vessels continue to branch and become smaller arterioles. Together, the small arteries and arterioles represent the primary vessels that are involved in regulating arterial blood pressure and blood flow within the organ. These vessels are highly innervated by autonomic nerves (particularly sympathetic adrenergic), and respond to changes in nerve activity and circulating hormones by constricting or dilating. Therefore, these vessels are referred to as resistance vessels. As arterioles approach 10 microns in diameter, they lose their smooth muscle to become capillaries, and comprise endothelial cells and a basement membrane. Capillaries represent the smallest vessels within the microcirculation and are the primary exchange vessels within the body. Across the capillary endothelium, oxygen, carbon dioxide, water, electrolytes, proteins, metabolic substrates and by-products (e.g., glucose, amino acids, lactic acid), and circulating hormones are exchanged between the plasma and the tissue space surrounding the capillary (interstitium). When capillaries join, they form postcapillary venules, which also serve as exchange vessels, particularly for macromolecules and fluid. As postcapillary venules join and form larger venules, smooth muscle once again appears. These venous vessels, like the resistance vessels, can dilate and constrict, and serve an important function in regulating capillary pressure. Venules form larger veins that serve as the primary capacitance vessels of the body - i.e., the site where most of the blood volume is found and where regional blood volume is regulated. For example, constriction of the veins decreases venous volume and increases venous pressure, which alters cardiac output. The final venous vessels are the inferior and superior vena cava, which carry the blood back to the right atrium of the heart.
The aorta, besides being the main vessel to distribute blood to the arterial system, dampens the pulsatile pressure that results from the intermittent outflow from the left ventricle. The actual dampening is a function of aortic compliance. Large arteries branching off the aorta (e.g., carotid, mesenteric, renal arteries) distribute the blood flow to specific organs. These large arteries, although capable of constricting and dilating, play only a small role in regulating pressure and blood flow under normal physiological conditions. Once a large artery reaches the organ it supplies, it branches into small arteries that distribute blood flow within the organ. These vessels continue to branch and become smaller arterioles. Together, the small arteries and arterioles represent the primary vessels that are involved in regulating arterial blood pressure and blood flow within the organ. These vessels are highly innervated by autonomic nerves (particularly sympathetic adrenergic), and respond to changes in nerve activity and circulating hormones by constricting or dilating. Therefore, these vessels are referred to as resistance vessels. As arterioles approach 10 microns in diameter, they lose their smooth muscle to become capillaries, and comprise endothelial cells and a basement membrane. Capillaries represent the smallest vessels within the microcirculation and are the primary exchange vessels within the body. Across the capillary endothelium, oxygen, carbon dioxide, water, electrolytes, proteins, metabolic substrates and by-products (e.g., glucose, amino acids, lactic acid), and circulating hormones are exchanged between the plasma and the tissue space surrounding the capillary (interstitium). When capillaries join, they form postcapillary venules, which also serve as exchange vessels, particularly for macromolecules and fluid. As postcapillary venules join and form larger venules, smooth muscle once again appears. These venous vessels, like the resistance vessels, can dilate and constrict, and serve an important function in regulating capillary pressure. Venules form larger veins that serve as the primary capacitance vessels of the body - i.e., the site where most of the blood volume is found and where regional blood volume is regulated. For example, constriction of the veins decreases venous volume and increases venous pressure, which alters cardiac output. The final venous vessels are the inferior and superior vena cava, which carry the blood back to the right atrium of the heart.
The relative sizes and functions of different blood vessels are summarized in the following table:
| VESSEL TYPE | DIAMETER (mm) | FUNCTION |
| Aorta | 25 | Pulse dampening and distribution |
| Large Arteries | 1.0 - 4.0 | Distribution of arterial blood |
| Small Arteries | 0.2 - 1.0 | Distribution and resistance |
| Arterioles | 0.01 - 0.20 | Resistance (pressure & flow regulation) |
| Capillaries | 0.006 - 0.010 | Exchange |
| Venules | 0.01 - 0.20 | Exchange, collection, and capacitance |
| Veins | 0.2 - 5.0 | Capacitance function (blood volume) |
| Vena Cava | 35 | Collection of venous blood |
Distribution of Pressures and Volumes
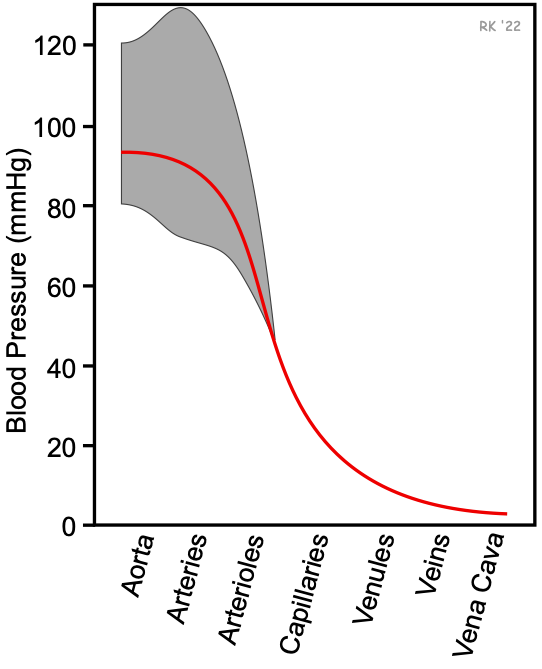 As shown in the figure, the aorta and arteries have the highest blood pressure. The mean aortic pressure (solid red line) is about 90 mmHg in a resting individual with normal arterial pressures. The mean blood pressure does not fall very much as the blood flows down the aorta and through large distributing arteries. It is not until the small arteries and arterioles that there is a large fall in mean blood pressure. Approximately 50-70% of the pressure drop along the vasculature occurs within the small arteries and arterioles because of their large contribution to systemic vascular resistance. By the time blood reaches the capillaries, the mean pressure may be 25-30 mmHg, depending on the organ. The pressure falls further as the blood travels into the veins and back to the heart. Pressure within the thoracic vena cava near the right atrium is very close to zero and fluctuates from a few mmHg negative to positive with respiration.
As shown in the figure, the aorta and arteries have the highest blood pressure. The mean aortic pressure (solid red line) is about 90 mmHg in a resting individual with normal arterial pressures. The mean blood pressure does not fall very much as the blood flows down the aorta and through large distributing arteries. It is not until the small arteries and arterioles that there is a large fall in mean blood pressure. Approximately 50-70% of the pressure drop along the vasculature occurs within the small arteries and arterioles because of their large contribution to systemic vascular resistance. By the time blood reaches the capillaries, the mean pressure may be 25-30 mmHg, depending on the organ. The pressure falls further as the blood travels into the veins and back to the heart. Pressure within the thoracic vena cava near the right atrium is very close to zero and fluctuates from a few mmHg negative to positive with respiration.
The arterial pulse pressure (shown as the gray band around the mean pressure in the figure) increases as the blood flow travels down the aorta and into distributing arteries. The systolic pressure rises and the diastolic pressure falls, therefore the pulse pressure increases. This occurs because of reflective waves from vessel branching and from decreased arterial compliance (increased vessel stiffness) as the pressure pulse travels from the aorta into distributing arteries. As the blood flows into smaller arteries and arterioles, the pulsatility declines.
Regarding the distribution of blood volume within the circulation, the greatest volume is found in the venous vasculature, which contains 60-80% of the blood volume. For this reason, veins are referred to as capacitance vessels. The relative volume of blood between the arterial and venous sides of the circulation can vary considerably depending upon total blood volume, intravascular pressures, cardiac output, vascular resistance, and vascular compliance.
Cardiac output and systemic vascular resistance undergo large changes with physical activity, and these changes result in a redistribution of pressures and volumes, as well as blood flow, within the circulatory system.
Revised 02/01/2024

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)