Factors Regulating Arterial Blood Pressure
Mean arterial pressure is regulated by changes in cardiac output and systemic vascular resistance. The following scheme summarizes the factors that regulate cardiac output and systemic vascular resistance.
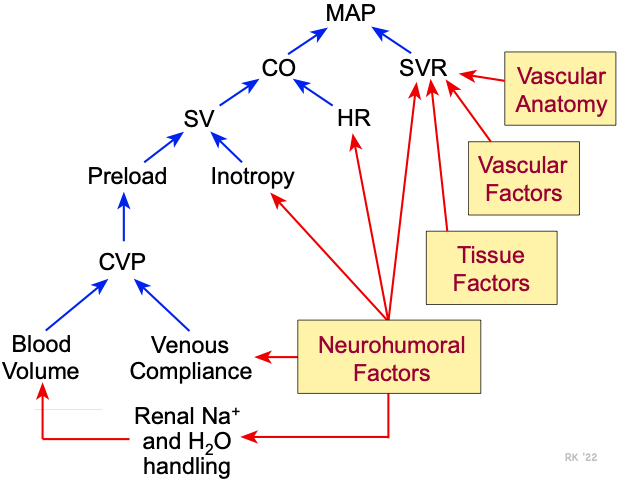 Cardiac output is determined by the product of stroke volume and heart rate. Stroke volume is determined by inotropy and ventricular preload. (The effects of afterload on stroke volume are not shown in this figure.) Ventricular preload is altered by changes in central venous pressure, which is altered by changes in venous compliance and blood volume. A decrease in venous compliance as occurs when the veins constrict, or an increase in blood volume increases ventricular preload by increasing central venous pressure. Total blood volume is regulated by renal function, particularly the renal handling of sodium and water. Blood volume shifts within the body (not shown in figure) as occurs when changing body posture, also change central venous pressure and preload. Heart rate, inotropy, venous compliance, systemic vascular resistance and renal function are all strongly influenced by neurohumoral mechanisms.
Cardiac output is determined by the product of stroke volume and heart rate. Stroke volume is determined by inotropy and ventricular preload. (The effects of afterload on stroke volume are not shown in this figure.) Ventricular preload is altered by changes in central venous pressure, which is altered by changes in venous compliance and blood volume. A decrease in venous compliance as occurs when the veins constrict, or an increase in blood volume increases ventricular preload by increasing central venous pressure. Total blood volume is regulated by renal function, particularly the renal handling of sodium and water. Blood volume shifts within the body (not shown in figure) as occurs when changing body posture, also change central venous pressure and preload. Heart rate, inotropy, venous compliance, systemic vascular resistance and renal function are all strongly influenced by neurohumoral mechanisms.
Systemic vascular resistance is determined by the anatomy of the vascular network (series versus parallel resistance elements) and by the state of vascular tone. Anatomic structure remains relatively unchanged in healthy adults; however, pathological conditions (e.g., vascular thrombosis) can affect the number of perfused blood vessels. Changes can occur in the relative number of parallel and series resistance elements. In hypertension, there is evidence that rarefaction occurs, a decrease in the anatomical number of arterioles and capillaries. In response to exercise training, new parallel vessels can develop in muscle tissue.
The most important mechanism for changing systemic vascular resistance involves changes in vessel lumen diameter (i.e., changes in vascular tone). The Poiseuille relationship shows that resistance is inversely related to the fourth power of the vessel radius. In chronic hypertension, vessel radius is often reduced because of a thickening of the vessel wall - this leads to a reduction in lumen size. Vascular factors such as nitric oxide, endothelin, and prostacyclin have important influences on vessel diameter. Myogenic mechanisms intrinsic to the vascular smooth muscle also can alter vessel diameter. Tissue factors (e.g., adenosine, potassium ion, hydrogen ion, histamine) are chemicals released by parenchymal cells surrounding blood vessels that significantly alter vessel diameter. Tissue factors are more important for regulating organ blood flow than systemic arterial pressure; however, changes in vessel tone can affect both organ blood flow and systemic arterial pressure. Finally, neurohumoral mechanisms play a significant role in regulating systemic vascular resistance and arterial pressure, particularly in certain forms of secondary hypertension. Neurohumoral mechanisms are regulated principally by arterial baroreceptors and, to a lesser extent, by chemoreceptors. Many of the therapies used for reducing arterial pressure involve inhibiting the action of neurohumoral mechanisms.
Revised 12/7/2022

 Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021)
Cardiovascular Physiology Concepts, 3rd edition textbook, Published by Wolters Kluwer (2021) Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)
Normal and Abnormal Blood Pressure, published by Richard E. Klabunde (2013)